In October 2021, Dawn Holt felt a lump in her right breast as she bent over to pick something up. Taking action immediately, she spent the next year battling breast cancer and has successfully completed her treatments. Now, she’s telling women to listen to their body.
By Charlotte Stefanski, cstefanski@iuhealth.org, writer for IU Health’s Indianapolis Suburban Region
It was a Friday evening in October 2021, and Dawn Holt was catching up on some TV. She remembers dropping something on the floor, and when she bent over to pick it up, she felt something unusual.
When her breast rubbed against her arm, the then 39-year-old could feel a lump. It wasn’t rock hard, but it was distinctive.
Since it was a Friday, she had an entire weekend to mull over what the lump could be, but already, Holt had a plan to call IU Health University Hospital and schedule a mammogram as soon as possible.
“Literally, my life changed the moment that I reached down to pick up the remote control,” Holt said. “My intuition is very strong and I knew that it wasn’t nothing.”
A few days later, she was able to go in for her mammogram and ultrasound, and during the procedure, the radiologist let Holt know she had concerns about what she was seeing.
While the news was scary, it was also a little reassuring, Holt explained. She’s a planner, and hearing that her intuition was right and that she might have to do more tests let her think ahead.
“Even though so much of this journey has been so out of my control, that aspect of it was comforting,” she said.
Holt was scheduled for a biopsy, and once her results came back, it was confirmed—she was diagnosed with estrogen receptor positive right breast cancer.
Her year-long treatment plan would begin a few weeks later, with Holt making plans to fight her cancer at IU Health North, University and West hospitals.
Forming an aggressive treatment plan
Luckily, Holt had caught it early, and she had a few ways she could go about treatment. A friend of hers had attended the Indiana University School of Medicine, so already, she had an idea for who she wanted as her breast surgeon and oncologist.
Things moved quickly after her official diagnosis. Holt began meeting with her breast surgeon, medical oncologist and radiation oncologist during the last week of October 2021 and then had her first chemotherapy treatment on Nov. 8.

“My phone was just ringing off the hook. It was IU Health; where do I need to be, what’s happening?” Holt said. “I was very clear. I would go to any facility. This needed to be my priority.”
Holt opted to go with a more aggressive approach to treatment, with chemotherapy first at the IU Health Simon Cancer Center in downtown Indianapolis. It included eight weeks of one type of chemo regimen, followed by another 12-week medication.
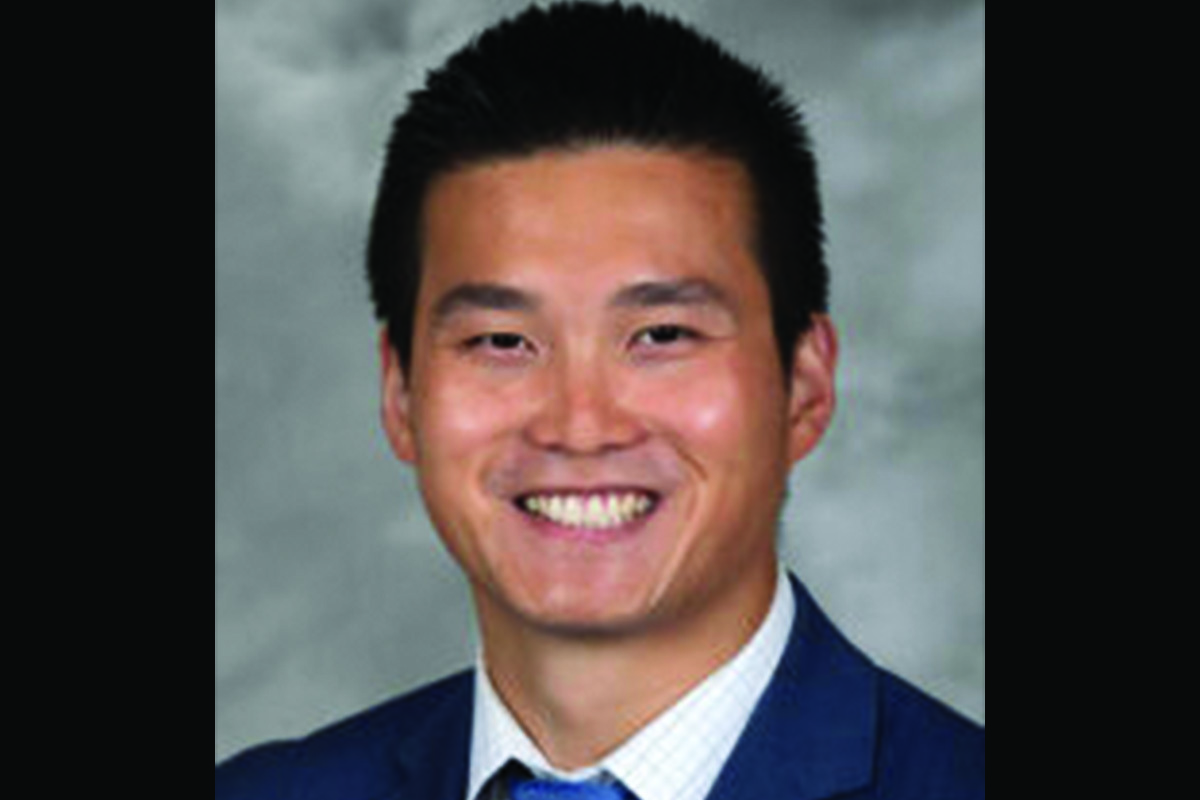
“We are fortunate at IU Health to have a multidisciplinary tumor board at each of our breast treatment sites. Dawn’s case was reviewed in tumor board and given the features of the disease we felt the best intervention to initiate her treatment was chemotherapy,” said Dr. Sade Imeokparia, Holt’s breast surgeon. “Chemotherapy upfront can give an advantage in certain circumstances, and when this is recommended, it is not to be taken lightly. Any chemotherapy is daunting and the whole course can be very precarious.”

One of the reasons Holt decided to complete chemotherapy first at the IU Health Simon Cancer Center was because her medical oncologist, Dr. Kathy Miller, could tell if it was working. During breast exams, she could already tell the lump was shrinking.
“Chemo is very hard. It’s physically hard, but also mentally and emotionally draining,” Holt explained. “Having those appointments where she was like, ‘It’s definitely shrinking,’ helped me to continue on.”
Once chemotherapy came to an end, Holt then scheduled a right-sided mastectomy with Dr. Imeokparia at the IU Health Joe & Shelly Schwarz Cancer Center in Carmel this April.
Dr. Imeokparia met Holt after returning from maternity leave and remembers that while Holt could be quiet at times, she was always a warm and bright spirit when coming into Schwarz Cancer Center.
“In the first moments of meeting her, her infinitely huge heart came shining through. I can’t say enough about how it is remarkably invigorating for me as a person and clinician to get to know a patient as a person as well, beyond their diagnosis,” Dr. Imeokparia said. “I also had the pleasure of getting to meet her family. Dawn has a fantastic support system in her family and their love for her is abundantly clear.”
Since genetic testing came back negative and Holt had no family history of breast cancer, she decided to only do the right side and plans to get an implant later on.
“The left one hasn’t done anything wrong. I don’t want to punish it,” she joked.
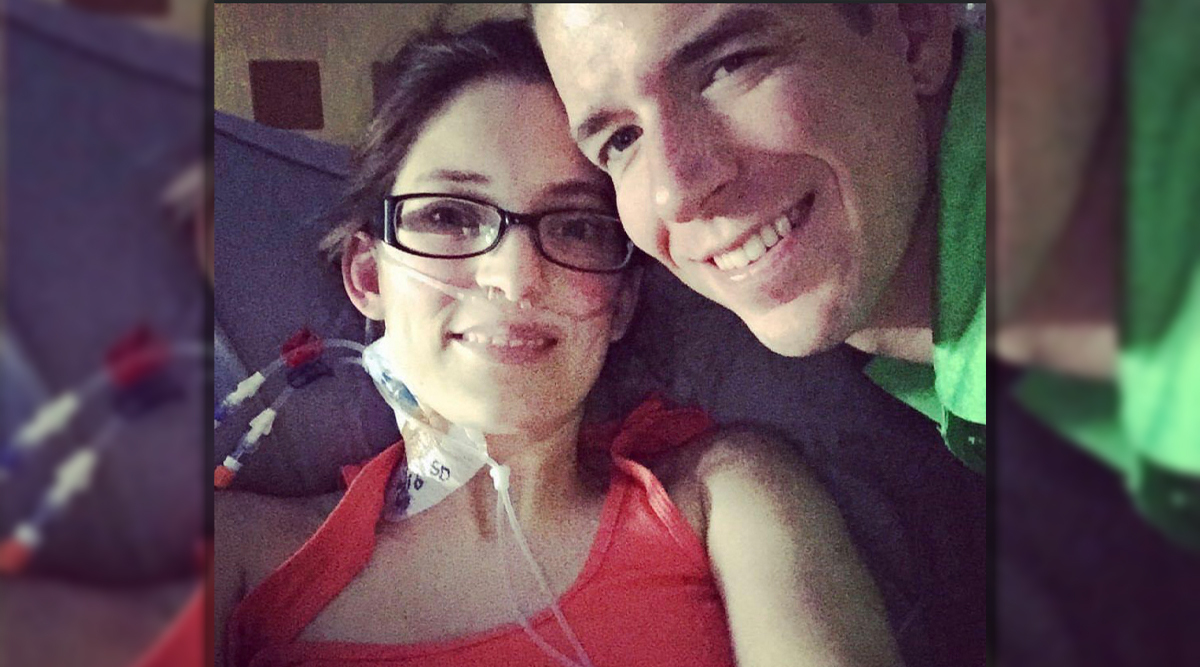
Her surgery included placing a tissue expander for the breast reconstruction procedure, but Holt’s body ended up rejecting it in the form of a pseudomonas infection. After the expander was taken out, Holt needed time to heal and treat her infection.
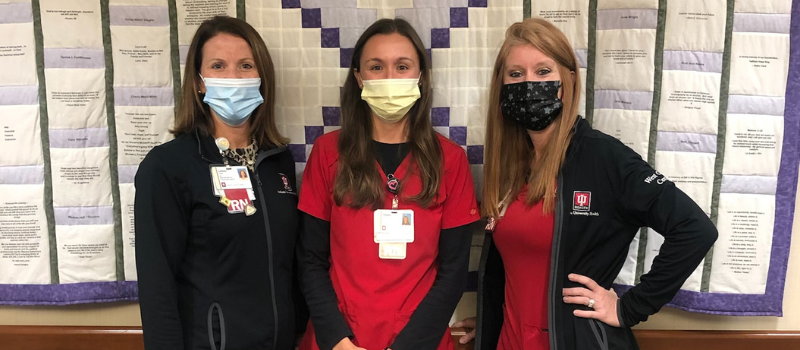
Once everything was clear, she began her radiation treatments at the IU Health West Cancer Center with her radiation oncologist, Dr. Paul Anthony.
She wrapped up treatment this September and will soon begin hormone therapy. Right now, her scans are clear and Holt is cancer free.

Through her year-long battle, faith has been a constant in Holt’s life and one of the reasons she was able to make it through, whether it be singing at church, going to a Bible study class or even doing administrative work.
Her support system was also crucial, including both her father and the Pink-4-Ever organization, which connected her to other breast cancer survivors during her journey. Holt was also transparent about her cancer on social media, documenting her journey along the way. She not only received support from friends and family that way, but from complete strangers as well.
“I thought maybe this will encourage somebody else,” she said. “This is a way for me to document things too, so that if people do ask me questions, I can look through my social media and find things.”
‘Listen to your body’
Currently, Holt has follow-up appointments scheduled with both her medical and radiation oncologist, and she’ll soon have another mammogram with her left breast during her annual survivorship appointment.
October is Breast Cancer Awareness Month and Holt advises women to pay attention to their bodies, no matter their age. With no family history of breast cancer, Holt wouldn’t have had her first mammogram until age 40, which would have been March of this year.
She knows her outcome could have been completely different if she hadn’t discovered the lump.
“Get your screenings, get your mammogram. It’s not comfortable, but it’s so important. We get so busy with life, and so many women are wives and mothers, and have a career and all these things that they’re juggling,” Holt said. “But I would just remind them that they can’t take care of anyone else if they’re not here and not well to do so. It’s so important to prioritize taking care of our own health.”
Like with any cancer, Dr. Anthony said that early detection is crucial. For breast cancer, that means scheduling a mammogram.

“The only way to do that is with a mammogram, which will result in a higher level of care, and less need for toxic treatment regimens,” he said. “If we find it really early, then you might not need chemotherapy; you usually just need surgery, maybe combined with radiation. That’s the big benefit.”
Dr. Anthony also noted that generally, the start age for an annual mammogram is 40 years old, but for women with a family history of breast cancer, the recommended age is 30 – 35. IU Health recommends women should meet with their primary care provider to discuss their level of risk for breast cancer and when it would be best for them to start getting mammograms. Each person is different and requires a personalized approach to their screening care.
“Women should be aware that breast cancer is indiscriminating. Screening mammograms are evidence-proven to help detect disease early, which can help improve outcomes significantly,” Dr. Imeokparia added. “Nevertheless, mammograms are not preventative. My best advice is to be proactive, and if you have dense breast tissue, strongly consider obtaining supplemental imaging beyond your yearly mammogram.”
Between IU Health University, North and West hospitals, Holt wants to thank her teams for their care.
“Every single person that I have encountered on this journey, whether it was the person scheduling appointments for me, whether it was the nurse that I called because I have a question, every doctor, every medical assistant that took my vitals at my appointments, the nurses who took care of me when I was hospitalized with my infection… Every single person has been so phenomenal, so kind, and compassionate, empathetic, and patient. I am overwhelmingly grateful to each and every one of them.”