An infant lays lifeless on an exam table inside a hospital emergency room. The mother tells the doctor that the baby had been fighting flu-like symptoms and is now struggling to breathe.
In another room, a 6-year-old drowning victim goes into cardiac arrest, the emergency room filled with a doctor and nurses scrambling to bring the child to life.
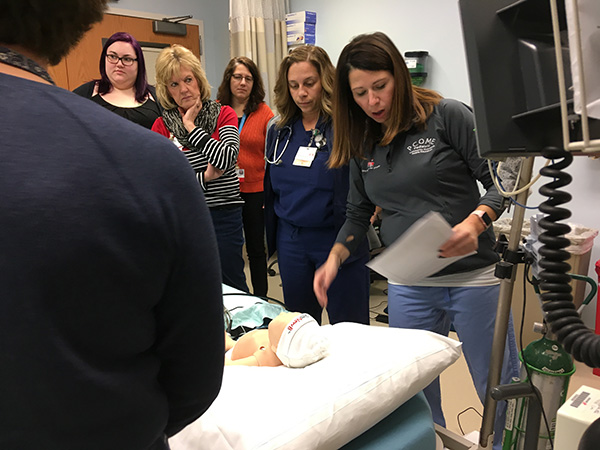 The emergency situations took place at Hancock Regional Hospital and the patients were mannequins, but the responders were real emergency room physicians and nurses. They were working alongside their peers from LifeLine and Riley Hospital for Children at IU Health. The exercise was part of The Pediatric Community Outreach Mobile Education (PCOME) training program.
The emergency situations took place at Hancock Regional Hospital and the patients were mannequins, but the responders were real emergency room physicians and nurses. They were working alongside their peers from LifeLine and Riley Hospital for Children at IU Health. The exercise was part of The Pediatric Community Outreach Mobile Education (PCOME) training program.
The goal of the program is to provide onsite training and expertise to community hospital healthcare providers in Indiana for the initial stabilization and management of pediatric patients. The program focuses on pediatric care in commonly seen pediatric illnesses and low volume high acuity illness. The training is geared toward multidisciplinary teams in their own environment, using mannequins to refine and refresh their skills in a realistic way without risk to the patients.
Why is the training important? Nearly 83% of children are seen at non-children’s hospitals. About 70 percent of emergency rooms see 15 children a day. Almost a third of Indiana hospitals are located in rural or remote areas.
PCOME team members include nurses Michele Kirby, Erin Montgomery respiratory, therapist Kellie Leeper, and physicians Riad Lutfi, Samar Abu-Sultaneah, and Kamal Abulebda – all specializing in pediatric critical care. Upcoming training sites include Terre Haute Regional Hospital, IU Health West, Evansville Deaconess Hospital and Johnson Memorial Hospital.
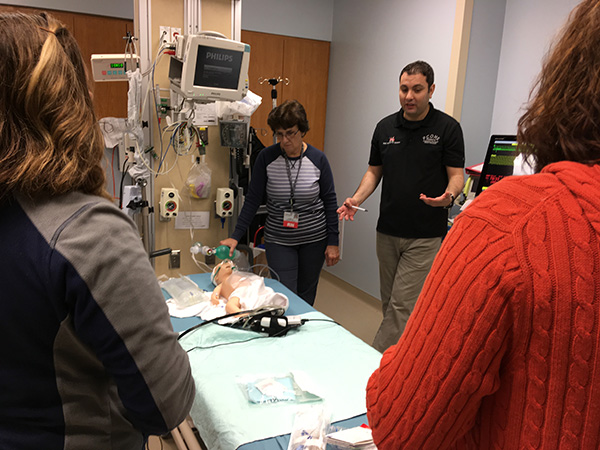 “As much as we try to mimic reality, we can’t get it perfect, but we tell them to take it seriously, because we want them to be prepared,” said Dr. Lutfi. During the training, mannequins display signs of distress from plummeted oxygen levels, to labored breathing. Staff members go through the emergency paces as if they were working on a real patient – ordering chest x-rays, administering CPR, and stabilizing the child for transport.
“As much as we try to mimic reality, we can’t get it perfect, but we tell them to take it seriously, because we want them to be prepared,” said Dr. Lutfi. During the training, mannequins display signs of distress from plummeted oxygen levels, to labored breathing. Staff members go through the emergency paces as if they were working on a real patient – ordering chest x-rays, administering CPR, and stabilizing the child for transport.
Taryn Papandria, who has worked as an ER doctor at Hancock Regional Hospital for 12 years said even though she knows she can call for an emergency transport to Riley Hospital, she also knows that minutes matter.
“We don’t see a lot of very sick children here, so having this refresher is important. If you don’t use it, you lose it. No matter how confident we are, it’s good to have outside resources come in to teach us.”
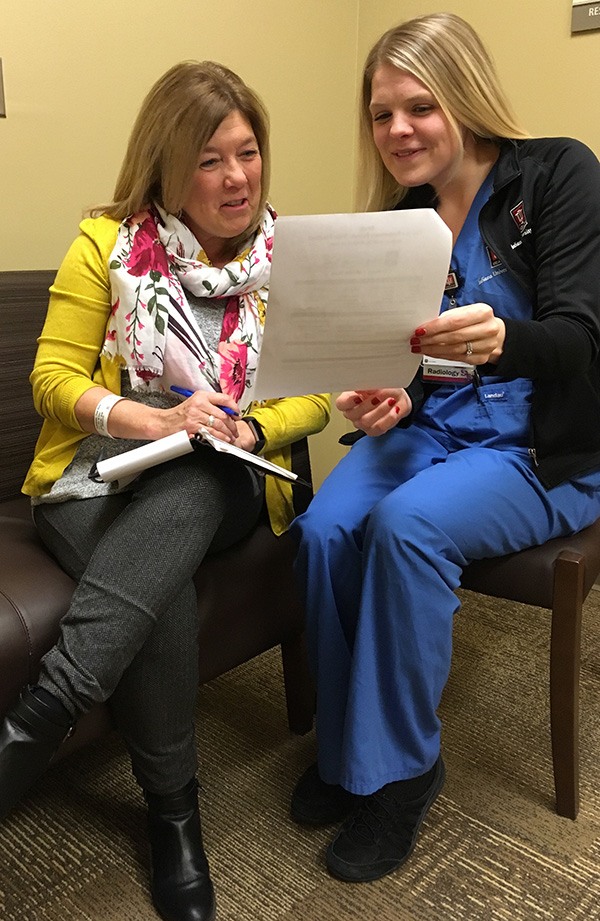
After each exercise, the PCOME team members ask the ER physicians and nurses to evaluate the care and outcome of the patient.
“Half the job with pediatric patients is determining how sick they are,” said Lufti. “It’s all about you. You are saving the kids’ lives.”
— By T.J. Banes, Associate Senior Journalist at IU Health.
Reach Banes via email at T.J. Banes or on Twitter @tjbanes.




 Here’s how it’s administered: You lie down on a flat surface (fully clothed), rest your arms above your head, and wait as the scan is completed. Four EKG stickers are attached to your left and right sides. You are asked to hold your breath for three sets of pictures. The first two times you hold your breath two to three seconds, the third time you hold your breath about five to seven seconds. The pictures are timed to your heart rate so that the technician can get the clearest scans possible.
Here’s how it’s administered: You lie down on a flat surface (fully clothed), rest your arms above your head, and wait as the scan is completed. Four EKG stickers are attached to your left and right sides. You are asked to hold your breath for three sets of pictures. The first two times you hold your breath two to three seconds, the third time you hold your breath about five to seven seconds. The pictures are timed to your heart rate so that the technician can get the clearest scans possible. “I’m not going to lie, I’ve made mistakes,” says Cornwell, who lives in Spencer, Ind. “So, there is bad news to tell. I went back to alcohol, which is what hurt me in the first place.”
“I’m not going to lie, I’ve made mistakes,” says Cornwell, who lives in Spencer, Ind. “So, there is bad news to tell. I went back to alcohol, which is what hurt me in the first place.” He says he has no side effects from the injury except for the short-term memory loss.
He says he has no side effects from the injury except for the short-term memory loss. 
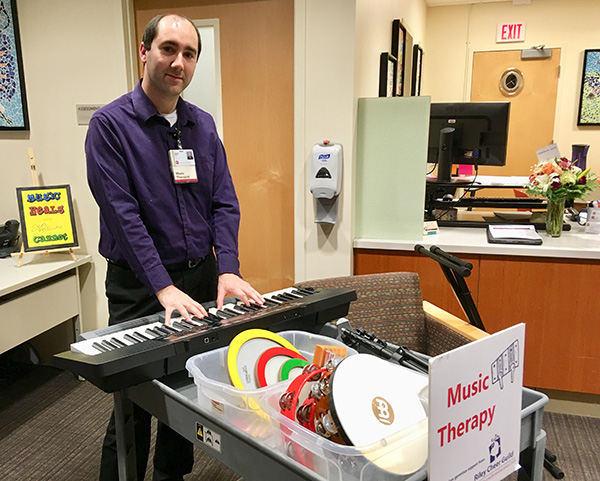 Those words became lyrics for Adam Perry’s impromptu song:
Those words became lyrics for Adam Perry’s impromptu song: