Methodist Hospital emergency nurse, Jessica Casse, offers an inside look at how patients are cared for at the busiest emergency department in the state of Indiana. “It can get very busy in here. It feels like organized chaos sometimes, but the main priority is always getting patients the care they need.”
Month: August 2023
Staying squeaky clean through the Fishers expansion
While construction won’t directly impact IU Health Saxony’s Central Sterile department for some time, its leaders are ensuring their team is engaged and informed throughout the whole process.
By Charlotte Stefanski, cstefanski@iuhealth.org, writer for IU Health’s Indianapolis Suburban Region
When visiting IU Health Saxony, most patients interact with those involved in their care, whether it be doctors, nurses, care assistants and more.
But there’s one department that has a huge impact on patient outcomes—even though they’re rarely seen on the main floors of the hospital.
Those in Central Sterile are responsible for cleaning, inspecting and sterilizing all surgical instruments and procedural equipment.
“We help a lot with keeping the infection rate down, so it’s really important,” said Supervisor Stacy Reed-Borum.
Reed-Borum has 13 years of sterile processing experience. She joined IU Health in 2016 and came to IU Health Saxony—soon to be IU Health Fishers—four years ago. The department’s team lead, Chris Goodling, joined the team when Saxony first opened its doors in 2012.
Located in the lower level of the hospital, those working in Central Sterile not only meticulously clean the instruments, but they have plenty to memorize as they prepare the needed tools for different procedures.
“I didn’t even know Central Sterile existed until I came here,” Goodling said. “It’s very interesting. A lot of learning, but it’s fun to do.”
Involved since Day 1
When the Fishers Community Impact Project was announced in 2022, Reed-Borum was a little apprehensive.
The $300 million investment would include a significant expansion of the IU Health Saxony Hospital campus, adding more beds and several new services, including pediatric emergency medicine and obstetrics and gynecology.

While it was exciting for her community and fellow team members, she was unsure how it would impact her department’s work and wellbeing. In her 13 years in healthcare, Reed-Borum knew that Central Sterile could sometimes be left out of conversations when it came to things like facility expansions.
However, that wasn’t the case at IU Health Saxony.
“Architects came down before any plans were made and asked us what we would need if we had ‘x’ number of patients,” Reed-Borum recalled. “I’m thankful that we’ve been included since day one. We get updated weekly on the progress of the expansion.”
That feeling of inclusion has helped the department embrace the change and have excitement as construction continues.
For Goodling, a Fishers resident, that excitement has been a longtime coming. He’s watched the area grow rapidly and saw the need for expanded services at the hospital.
“It’s been really cool to see all of the buildings, and then to be part of Saxony from the very beginning,” Goodling said. “To seeing where it’s going is really cool.”
Future impacts on Central Sterile
Now more than a year into the expansion, the hospital is currently experiencing heavy construction in its Emergency department, Imaging and Short Stay units.
Central Sterile won’t be directly impacted by the construction until the end of the project, which is slated to wrap up in 2025. But already, the team is gearing up for changes.
“Even right now, we’re trying to change certain ways of how we’re doing things—trying to prepare how we’re going to move into the department,” Goodling said.

More patient beds and new services means that Central Sterile will have an increase in the number and types of tools the department works with. Up until this point, the team has worked mostly with tools related to orthopedic procedures.
“That’s exciting for us because we see mostly orthopedic cases. Now, we have pediatric emergency medicine and general surgery, and we added in labor and delivery too,” Reed-Borum said. “It makes us feel like we’re doing even more for the community than just surgery.”
While Central Sterile expands, it will remain in the same location of the hospital. And similarly to other departments, the team will also have the chance to participate in “day-in-the-life” activities, where team members test out their new surroundings and make adjustments.
Goodling is excited for upgrades that come along with the construction, including a new generator and steam line—both of which will help cleaning and sterilization power.
There will also be more space for team members to gather their tools, which Goodling explained would function like a grocery store aisle.
“I think it’s pretty exciting. We’re not patient facing, in fact, patients don’t even know we exist, but we play a really big role in their care,” Reed-Borum explained. “When somebody comes in the Emergency department (ED), we supply things to the ED. We also supply things to Cath Lab. So as those departments are growing and seeing more patients, we’re also seeing more patients.”
Keeping up as construction continues
While it will be some time before Central Sterile is directly impacted by construction, Reed-Borum and Goodling are ensuring their team stays informed and involved throughout the process.
Reed-Borum was pleasantly surprised by the smooth transition during the expansion, as she knows transitions like these can be hard, and she’s glad that care teams have been consulted.
“I thought it was really awesome that they came to us and said, ‘What do you need? How should this flow?’” she said. “There’s times where they’ve come to us with a blueprint, and we tell them why something won’t work, and then they change it to where it will work.”
Goodling added that being so involved has helped with morale, both for his team members and even the construction crews.
He knows his department will be a tricky construction zone in the future, as the instruments need to be kept clean and dust free, and those coming in and out will have to wear the surgical “bunny” suit.
In the meantime, they want to thank their construction partners.
“I want to give some kudos to the construction workers—the ones working inside and especially the ones working outside, because they’ve worked in some crazy weather to get this done,” Reed-Borum said. “They’re playing a big part in this too.”
One small surgery can make a huge difference
Going into surgery, Mary Stevenson, 74, was scared. Like many people, she hated needles. But she wanted to stop the pain in her finger that had caused her months of discomfort, so she went through with the 30-minute trigger finger release procedure.
Six months prior, Stevenson started to notice a pain in her right ring finger. She began to struggle to move the finger and lift it up. It was so bad she was at the point where she could barely even lift a heavy pan to cook dinner. After telling her doctor, she was referred to the orthopedics office at IU Health Ball Memorial Hospital to see Jacob Triplet, DO, a hand and upper extremity reconstruction specialist.
When she went to schedule her appointment, she was able to set up a time within the same week. At her first consultation, she met with Triplet and showed him what was wrong. When she tried to lift her finger, she felt an awful pain—the same pain she had been experiencing for weeks.
“He was so nice,” said Stevenson. “He explained things in normal people’s language, instead of all doctor stuff.” He told me what they would do and what would happen. He checked in and made sure I felt comfortable with the procedure.”
Triplet diagnosed Stevenson with stenosing tenosynovitis, commonly known as trigger finger. Trigger finger is a common condition that more than 200,000 people report having a year. It occurs when the tendons that flex the fingers and thumbs become inflamed. This results in a stiff feeling in the finger and intense pain when you try to straighten or bend the finger, just like what Stevenson was experiencing.
After discussing the diagnosis, Triplet explained the treatment plan. He told Stevenson that he would perform a trigger finger release surgery, in which a small cut is made on the finger to allow the tight tendon to move freely without pain.
The surgery was performed while Stevenson was awake. Triplet made a tiny incision in the tissue over the sore tendon, just like he had explained during the consultation. He then gave her a few stitches and told her to return in three days for a check-up.
Stevenson said that although she was nervous, Triplet and his team put her at ease. “They were all so personable,” she said. “It made my experience memorable. When I went back, I was already able to move my finger and they took the stitches out. Within a week, I didn’t even know I had it. It was wonderful! Today, you can’t even tell that I have a scar anymore.”
After her surgery, Stevenson was able to go back to her normal life, which includes spending time with her husband, children, grandchildren and three great grandkids. Making holiday memories can continue, too. Every Christmas she and her husband make more than 600 cookies to share with friends and family, but last year she was concerned she wouldn’t be able to because of her trigger finger. With the help of Triplet and her care team at Ball, she is back to doing what she loves.
“I recommend Triplet to anybody that says, ‘I have a trigger finger and I don’t know what to do,’” Stevenson said. “Go to Dr. Triplet immediately. You’d be so surprised at how much of a difference there is. I was at the point where I couldn’t do much of anything. I had to get something done. And now, it’s wonderful.”
Helping families feed their babies
There’s no one-size-fits-all way to raise a strong, happy, healthy child. Every child and family has unique circumstances to navigate, including the question of how to feed your infant.
And if breastfeeding is your choice, having the necessary resources is essential.
Linda Ebright, CNM, with IU Health Southern Indiana Physicians OBGYN, knows first-hand how common it can be for individuals to struggle with breastfeeding, especially initially.
“Yes, it is important to feed the baby, and we’re all thankful for donor milk and formula when needed,” says Ebright. “But if a person chooses to breastfeed, they should be able to access the resources they need to hopefully be successful, and their values and desires should be central to the care plan.”
The list of benefits to breastfeeding continues to grow, which makes it all the more important to help those who want to breastfeed their children. Research has shown that these benefits include:
- Providing babies with their nutritional needs
- Protecting babies from illnesses and helping build their immune systems
- Decreased ear infections and hospitalizations as babies
- Lower rates of obesity and diabetes when they grow into adulthood
- Some cancers, type 2 diabetes and high blood pressure are less common in women who breastfed their children
“As a lactation consultant, there were times I would work with people who wanted to exclusively breastfeed their babies so badly, but struggled to make enough milk, or perhaps had latch issues that prevented that from happening,” says Ebright. “This can be so hard, emotionally.”
It’s important to remember that giving a baby any amount of breast milk can be helpful since each teaspoon is full of living immune cells. Ebright also likes to share with parents an anecdote she once heard, “Kindergarten teachers cannot tell which kids were breastfed, but they can tell who was read to as a small child.”
“There are so many important aspects to the parent-child bond, and you can be a really amazing parent and have a strong bond with your child without exclusive breastfeeding,” says Ebright. “This also applies to people who may not want to breastfeed at all.”
She continues to explain how it’s essential to support families where they are. Sometimes, a person’s past experiences or current resources can impact what they can or want to do.
“But if someone wants to breastfeed, we want to help them be as successful as possible in meeting their goals,” she says.
There is help in the community, including IU Health Bloomington lactation consultants, La Leche League, Milk Matters, local WIC offices and local obstetric offices.
“When talking about breastfeeding to pregnant and postpartum people, the most important message that I want them to hear is that there is help,” says Ebright. “It’s not uncommon to struggle with breastfeeding at first, but many people in this community want to help you work through these challenges.”
Nurse spotlight: Grace Huizinga
After Grace Huizinga graduated from nursing school a little more than a year ago, she decided to jump in with both feet, getting her first job in Methodist Hospital’s emergency department. “It’s a lot and It’s been a really big adjustment [from school]. Thank goodness we have a good team here. There are a lot of skilled people here that you can learn from really quickly. You kind of have to learn quickly because it’s so fast paced.”
Heartfelt gratitude: IU Health Tipton’s cardiology team saved husband and wife
By Emma Avila, epackard1@iuhealth.org, writer for IU Health’s Indianapolis Suburban Region
IU Health Tipton’s cardiology team played a crucial role in saving the lives of Roger and Jennifer West.
Roger and Jennifer West just celebrated their 20th wedding anniversary with a vow renewal. They love going on day trips, antiquing and participating in 5K runs. They tell people that they’re able to do all the things they love thanks to the team at IU Health Tipton.
Both are patients of Dr. Nathan Lambert, cardiologist, and Beverly Altman, cardiology nurse practitioner. Altman works in collaboration with Lambert and his partners at both the IU Health Tipton and IU Health Saxony in Fishers. She is part of a team-based approach to ensure timely access to high quality cardiology services for both acute and chronic patient care and concerns.
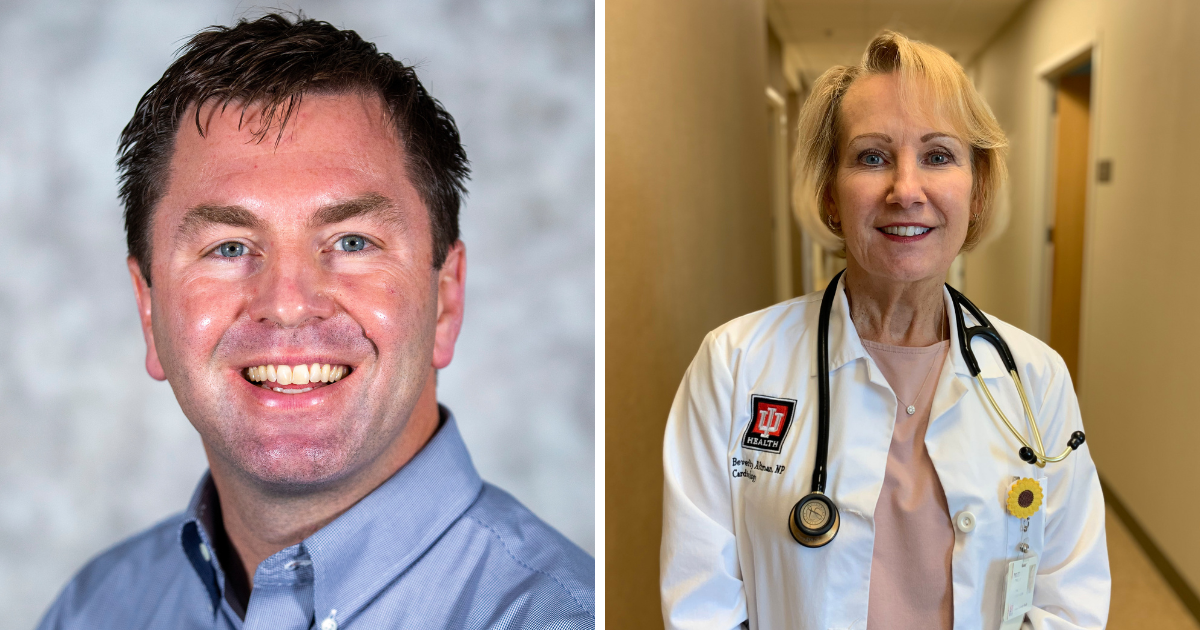
“I see patients independently. They are also patients of the group, but they can see me on a regular basis. If there aren’t any significant concerns, I can treat them,” Altman explained. “I think patients often feel comfortable coming to us with concerns. It helps with the completeness of the care.”
“Having a nurse practitioner like Beverly is essential to our practice,” Lambert added. “We have a large practice with offices in both Tipton and Hamilton counties, and neither one of us could see all the patients alone. Beverly is my right hand. I trust her completely and patients do too. She is the ultimate professional, reviews every chart in detail before each visit and follows through on every issue after the visit, big or small. She does what she says she will do, and patients value that.”
Roger began seeing the duo in 2017 due to the onset of atrial fibrillation, or AFib. If you have AFib, your heartbeat can be fast, chaotic and irregular. It can lead to blood clots, stroke or heart failure because your heart isn’t pumping blood like it should. With medication, Roger was able to get this under control.
In early 2022, he had vascular procedures performed on both legs at another facility. He followed up with Altman, who reviewed the notes and thought it would be wise for Roger to get a coronary calcium scan.
“Normal results should be zero. His was 4,000,” she explained.
After that, Altman recommended a stress test to check for blockages in the heart as well. The results came back abnormal.
Altman took the results to Lambert and recommended a heart catheterization. Lambert agreed, and he performed the catheterization at IU Health Saxony in August of 2022. They found significant blockages. The next step was bypass surgery at IU Health Methodist in September.
“I’m doing wonderful now. My heart is as strong as can be,” Roger said. “It was because Beverly took the time to go over everything and not just try to whisk me out of the office like a lot of health care professionals do. She actually saved my life.”
Roger isn’t alone in that gratitude. His wife Jennifer began seeing Lambert and Altman in 2019 for uncontrolled hypertension, tachycardia and difficult to control premature ventricular contractions.
Altman ordered blood tests, which included tests for Jennifer’s thyroid numbers.
“The tests came back, and my thyroid number was very low,” Jennifer explained. “Beverly sent the information over to my doctor, and I was set up with an ultrasound of my thyroid. Come to find out, I had a lesion that started midline and went to the left, along with several nodules.”
After surgery in March of 2022 to remove Jennifer’s thyroid, she found out she did have thyroid cancer.
“If it weren’t for Beverly paying attention to my symptoms and listening to me, I’m not sure I’d still be here,” Jennifer said.
The surgery also helped with the other heart-related issues she was experiencing.
“Once Jennifer’s thyroid disease was discovered and effectively treated, her chronic cardiology abnormalities improved or resolved altogether,” Altman said.
The Wests are thankful Altman, Lambert and the entire team were thorough in their care and treatment.

“All I can say is praise God for Beverly,” Roger said. “She is a major asset to Dr. Lambert’s staff and a huge credit to why IU Health Cardiology is the best. Without her being at the top of her craft, I would not be here today.”
“We can’t say enough about Beverly,” Jennifer agreed. “She really wants to help and she does care.”
Lambert is also grateful to have Altman on the team, helping care for patients.
“She and I have worked together over 10 years now, so we communicate very well. It’s truly collaborative.” He added, “Beverly is not allowed to retire before I do.”
Chaplains, congregations join hands to help minister to those facing substance misuse
An innovative partnership is reaching out to Hoosiers 50 and older to offer substance abuse prevention and mental health services.
By TJ Banes, IU Health Senior Journalist, tfender1@iuhealth.org
Improved health doesn’t start and end at the hospital. Where people live, work, play, and worship are increasingly playing a role in their quality of life.
To help bridge the gap between hospital and home, IU Health initiated a program called, “Congregational Care Network” (CNN). More than two dozen congregations in Marion and Monroe Counties have trained volunteers to visit patients after they have been discharged from the hospital. Through regular contact, the volunteers provide a social aspect that may otherwise be missing from patients’ daily lives.
Now, that network has expanded to specifically assist residents 50 and older, facing substance misuse and mental health challenges.
“We’ve tried to identify congregations who have experienced working with people with mental health and substance misuse issues,” said IU Health Chaplain Greg Morse, who is overseeing the program. There are now three congregations in Marion County and one in Morgan County with members paired with those needing services.
“Most of the time we have referrals from our existing partnering congregations when we are looking to expand our program. This allows us to connect with congregations that have the knowledge and internal process to hit the ground running. Additionally, we have connected with organizations doing similar work such as the Wellness Connection in Marion County and Stability First in Morgan County. This offers an extra layer to the care,” said Morse. The Congregational Care Network was realized after so many people experienced the isolation related to the pandemic. As the program took flight, congregants identified other factors that needed to be addressed especially among the 50 and over population.
As connections are established those working in the community are equipped to provide awareness about substance abuse and education, treatment and prevention resources. Connectors listen to the patient’s concerns, help patients navigate the healthcare system and communicate patient concerns to providers. Congregational volunteers spend at least one hour a week talking to patients – either by phone or in person. The initiative is funded by a grant from the Indiana Family and Social Services Administration (FSSA).
“I’ve always had a caring nature and part of my ministry is wanting people to do well and have a healthy life,” said Morse, who has been with IU Heath for five years. Prior to that he pastored at a church on the westside of Chicago for nearly a decade.
“As I grew in the ministry, I wanted to be involved in programs that address the social determinants of health,” said Morse. Social determinants of Health (SDOH) are the non-medical factors that influence health outcomes. The US Department of Human Services lists five key areas of SDOH: Economic Stability, Education Access and Quality, Health Care Access and Quality, Neighborhood and Environment, and Social and Community.
A nurse is climbing mountains after pain intervention surgery
Brian Ison has worked at Indiana University Health Jay Hospital as a physical therapist for 25 years. As a supervisor for rehab services, he’s normally treating patients and improving their quality of life. But recently, he found himself on the receiving end of care.
In October 2022, Ison began to feel a surging pain in his hamstrings. “It was just one of those things where I was like, okay, I’m old. I’m just going to push through it. But it developed into shooting pain from the boney part of the butt all the way down to the mid part of the right hamstring. It became extremely painful.”
Ison follows a very active exercise regimen, walking, running or hiking six days a week. He believed that his hamstring strain was from an over-exertion of the muscle. To cope, Ison put his physical therapy knowledge to use, “I did a lot of stretching. I would modify the strengthening exercises and back off on the intensity of the workout.”
When Ison reached out to his primary care physician, he was told to continue doing his therapy exercises. The idea of an injection was mentioned, but not seriously considered.
“I was self-treating it for at least six to eight months with no relief. It got to the point where even sitting at work became painful, and I didn’t want to leave town because I knew I just couldn’t tolerate it. My family and I had planned for a big trip for the summer to go to the Upper Peninsula in Michigan. We were planning on hiking, biking, kayaking and driving. I knew I couldn’t go with the pain I was having. I knew I needed more than what traditional pain management could offer.”
When Ison discussed his pain and upcoming travel plans with his doctor, he was referred to Ankit Bhatia, DO. Bhatia is a pain medicine and anesthesiology physician at IU Health Ball Memorial Interventional Pain Services.
A few months later, Ison had his consultation with Bhatia. “I sat down with him and explained everything,” says Ison. Bhatia explained that an injection would help Ison’s condition. Even though it was an uncommon procedure Bhatia had done it before and Ison agreed to the surgery.
Bhatia performed a steroid based injection on Ison that helped to reduce the inflammation in the muscle. “It’s just like an anti-inflammatory medication that they were able to inject to the points of where the pain originates,” says Ison.
“They did it under fluoroscopy, or X-ray, so they are able to pinpoint exactly where the pain starts and inject the steroid with precision,” Ison says. “The procedure was done in the Ball outpatient surgery center. Bhatia had a physician assistant in radiology, nurses and techs to assist him. That was the main difference between Dr. Bhatia and the other doctors we have for traditional pain management. Interventional pain management is different than just pain management and pumps. He does a lot of injections that can more precisely intervene with the pain and stop it, while traditional pain management focuses more on how to work through the pain.”
The relief was almost instantaneous. That same day, Ison had a family trip planned to explore Gatlinburg, Tennessee. Ison was able to sit through the entire six-hour car ride and could join his family on the hiking excursions. “My quality of life is back to 100%. No problems whatsoever. I’m back to my normal fitness routine, sitting, able to go wherever, no limitations.”
Three months later, Ison was able to join his family on their planned vacation to the Upper Penisula. “It was just gorgeous, and I’m so thankful for the pain intervention options,” says Ison. “If we didn’t have the medical intervention, either we wouldn’t have made the trip at all, or if we did, we would have had to modify it, and wouldn’t have been able to do any of the hiking, kayaking and biking.
Ison has learned a lot from his experience at the surgery center, and he is now applying his knowledge to helping his own patients. “Having the ability to refer on to a specialist was something I needed to learn.” He says, “and since then, I’ve had several patients with similar types of pain, and I can now refer them to the same care plan I received.”
“If you’re not getting the results you are hoping for, have the conversation with your provider.” Ison advises, “there’s other options out there for you to improve your quality of life. Everybody feels like when they go to pain management, this is the last resort. They’re going to put me on long term narcotics, long term pain medications, it’s going to impact my life. Fortunately, there’s other options that interventional pain management can offer.”
From administrative assistant to practice administrator in four years
Lynda Knight has a knack for staying busy and always looking for career opportunities. She came to IU Health four years ago as an administrative assistant and has since advanced several positions to her current role as the practice administrator for the neurology department. “The IU Health way loves to see people grow.”
Meet the community health worker trying to reduce disparities in cardiovascular disease
Kristina Hargrove is a community health team member who manages the care of patients in the iHEART program, a collaborative aimed at reducing health inequities that contribute to heart disease. When patients with unmanaged high blood pressure come into the IU Health primary care office in downtown Indianapolis, Kristina invites them to join the program, which includes a free take-home blood pressure monitor as well as frequent text check-ins to talk about results. “We also see if the patients need help in the community as far as food insecurities, lack of transportation, discounts for medications, childcare, anything along those lines. If you need support with any of that, I’m here.”
