Chris Perrott says he’s a walking miracle. On April 18, 2023, he didn’t know if he’d walk out of IU Health Methodist Hospital ER.
By TJ Banes, Senior Journalist IU Health, tfender1@iuhealth.org
As he recently sat through an occupational therapy session, Chris Perrott shared the accident that brought him to IU Health. He also shared the progress that he never thought possible.
Perrott, 41, was 25 feet up a ladder, working on a dryer vent outside his Greenwood home when he lost his balance and fell to the ground. The father of two, was rescued by neighbors and transported by ambulance to IU Health Methodist Hospital. He remained hospitalized for eight days and was out of work in software sales for 10 weeks.
The injuries of that April 18, 2023 tragic accident included a broken back, ribs, and heavily fractured left wrist.
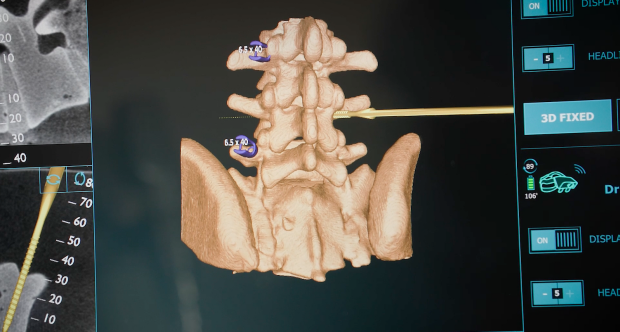
“I am very fortunate. When I was in ER the doctors and nurses said I could have been paralyzed or even dead. The good Lord was looking out for me,” said Perrott. He credits IU Health’s Dr. Jesse Savage for completing a spinal fusion that included placing two rods and screws in his back, and Dr. Anthony Archual for a successful hand surgery. Since May of 2023, he Perrott has been working with IU Health Occupational Therapist, Mamta Barmeda, who is certified in hand therapy and dry needling.
During a recent therapy session, Barmeda used Astym treatment to stimulate tissue growth, specifically with scar tissue in Perrott’s hand.
“When I first came out of the cast, she wanted me to try to touch all of my fingers with my thumb. I couldn’t do it,” said Perrott, demonstrating the progress. “We focus on specific areas each time. They’ve taught me the difference between a great recovery and a mediocre recovery. I am given exercises and I’m sticking with it,” said Perrott.
As he recovers, Perrott looks forward to coaching his kids’ sports and attending their activities.
“I’m now able to start jogging, and golfing is next. Every day is something new. Even walking up steps was a big thing. Cutting my meat with two hands was not a thing at all. The basics we take for granted were things I couldn’t do – playing catch, hitting baseballs and softballs and running up and down the basketball court – I just couldn’t do,” said Perrott.
“I am relieved and pleasantly surprised by the care I have received through IU Health,” he said. “You don’t know what you don’t know until you go through something like this. I’ve faced each day with the attitude of ‘what can I do next?’ and I appreciate all the guidance from the surgeons and therapists to keep me moving ahead.”